Russian Translation (download full abstract below):
Annotation of a scientific article on medicine and public health, the author of a scientific work is Trushova V.A., Alipenkova A.V.
A retrospective analysis of 39 case histories was performed for patients with breast pathology. All patients were divided into groups in accordance with the nosological form of the disease (fibrocystic mastopathy (PCM), fibroadenoma, breast cancer of various stages). Patients were fixed image of the iris with its subsequent sectoral analysis. A comparative analysis of the effectiveness of this method with the determination of its sensitivity and specificity. The method of detecting changes in the iris is effective in breast cancer in the early stages and prior to treatment.
ASSESSMENT OF THE OPPORTUNITY OF THE IRID DIAGNOSTICS METHOD INTEGRATED USE IN BREAST CANCER
A retrospective analysis of 39 case histories of patients with breast pathology was carried out. All patients were divided into groups (fibrocystic mastopathy (FKM), fibroadenoma, breast cancer of various stages). The image of the iris was fixed with sectoral analysis. The specificity of this method is carried out. It is a treatment for women.
Text of the scientific work on the topic “Assessment of the possibility of using the iridodiagnostics method in patients with breast pathology”
UDC 618.19-006.6-616-073
EVALUATION OF THE POSSIBILITY OF COMPLEX USING THE METHOD OF IRIDODIAGNOSTICS IN PATIENTS WITH BREAST PATHOLOGY Trushova V. A., Alipenkova A. V.
Scientific advisers – Zuy V.S. associate professor, cms; Soloviev V.I. Professor, Doctor of Medical Sciences; A. Borsukov, Professor, Doctor of Medical Sciences, Director, PNLI, Diagnostic Studies and Minimally Invasive Technologies; Semkina, Ye.N., Associate Professor, Ph.D.
FSBEI HE Smolensk State Medical University of the Ministry of Health of Russia
Russia, 214019, Smolensk, ul. Krupskaya, 28.
sgalaxy2 70615 @ gmail. com – Trushova Valeria Alexandrovna
Summary: A retrospective analysis of 39 case histories was conducted for patients with breast pathology. All patients were divided into groups in accordance with the nosological form of the disease (fibrocystic mastopathy (PCM), fibroadenoma, breast cancer of various stages). Patients were fixed image of the iris with its subsequent sectoral analysis. A comparative analysis of the effectiveness of this method with the determination of its sensitivity and specificity. The method of detecting changes in the iris is effective in breast cancer in the early stages and prior to treatment. Keywords: breast cancer, iridology
ASSESSMENT OF THE OPPORTUNITY OF THE IRID DIAGNOSTICS METHOD INTEGRATED USE IN BREAST CANCER
Trushova VA, Alipenkova AV
Doctor, Doctor of Medicine, Professor, Doctor of Medicine, Professor, Doctor of Medicine, Professor, Doctor of Medicine, Doctor of Medicine, Borsukov AV, Candidate of Medicine, assistant professor Semkina en
Smolensk State Medical University
28, Krupskoy St., Smolensk, 214019, Russia
sgalaxy270615@gmail.com-VA Trushova
Abstract. A retrospective analysis of 39 case histories of patients with breast pathology was carried out. All patients were divided into groups (fibrocystic mastopathy (FKM), fibroadenoma, breast cancer of various stages). The image of the iris was fixed with sectoral analysis. The specificity of this method is carried out. It is a treatment for women. Key words: breast cancer, iridology
Relevance. Early diagnosis of breast cancer (BC) remains today one of the most important problems in the world. The number of newly diagnosed cases of this pathology is steadily increasing. In Russia, there are about 45 thousand new cases annually [2]. Breast cancer is diagnosed in women older than 40 years in 90% of cases. Currently, the oncological service has a fairly powerful arsenal of diagnostic methods for verifying the diagnosis at the prehospital level (ultrasound, mammography, IHH) [4], but these methods cannot reveal a predisposition for breast cancer. There is a theory that by changes in iris stroma [1], namely the change in color tone, uniformity, the presence of lacunae, spots, ruptures of an autonomous ring (AK), indentations of AK, diffractions, it is possible to determine the presence of somatic pathology. The basis of the method of iridology is the principle of assessment of adaptive-trophic changes in the iris, which are associated with the negative projection-signal function of the nervous system. [5,6]. This method of diagnosis is controversial, is considered ineffective, but, nevertheless, there is a patent “Method for the rapid diagnosis of thyroid adenoma”, indicating a high diagnostic value of the proposed method [3].
The purpose of this work was to assess the possibilities of using iridodiagnostics in a complex diagnostic algorithm in patients with breast pathology.
Materials and methods. In 2017-2018 Smolensk Regional Oncology Clinical Dispensary (OGBUZ OOKD) and Problem Research Laboratory “Diagnostic Studies and Minimally Invasive Technologies” of Smolensk State Medical University analyzed the case histories of patients (n = 39) who were registered in OGBUZ DOCA from 2002 to 2017. The average age of patients was 59 ± 0.15 years. Iridology was performed by photographing in digital mode. Patients were examined by a single diagnostic algorithm, which included 2 stages:
Stage 1 – analysis of the history of the disease (physical examination, examination by an oncologist, complete blood count, biochemical blood test, mammography, chest X-ray, ultrasound of the mammary glands, conclusion of a pathologist on a tumor biopsy).
Stage 2 – fixing the image of the iris of patients with its subsequent sectoral analysis based on the criteria: the nature of the color tone, uniformity, density of the fibers of the iris in both eyes, the outer edge of the iris, the shape of pupillary border; study of the structure of the iris in the area of the projection of the breast. The search was carried out by the main iridoscale: lacunae, pigment spots, speckles, lymphatic rose garden (LR), “acidosis” – whitish plaque on the iris, tears, joint venture, indentation of AK, deflection.
Stage 3 – All patients were divided into groups, which are presented in Table 1.
Table 1. The distribution of patients by nosological groups of diseases
Diseases of the mammary gland Number of women (n) Middle age
FCM, fibroadenoma 5 53 ± 0.8
BI cancer (before surgery) 12 61 ± 0.58
Cancer B12 (before surgery) 17 56 ± 0.94
Cancer BO (before surgery) 1 67
RakB14 (after surgery) 4 50 ± 0.5
39 total
Stage 4 – a retrospective analysis of the treatment of 39 patients. Of these, patients with FCM (n = 3) and fibroadenoma (n = 2) underwent surgery — sectoral resection. Breast cancer patients received various types of treatment: surgical (mastectomy), chemotherapy (PCT), radiation therapy (RT), as well as a combination of these treatments. The distribution of patients with breast cancer by type of treatment is given in Table 2.
Table number 2. The distribution of breast cancer patients depending on the stage of the disease and treatment methods
Stage Surgical Surgical + PCT PCT PCT + LT Total
BI 12 – – – 12
Bg2 12 1 2 2 17
BOY – – – 1 1
Bg4 – 2 1 1 4
34 total
Iridology was performed in all patients according to the table №1.
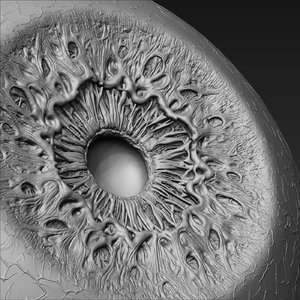
In the group of patients with PCM and fibroadenoma (n = 5), there is an accumulation of the largest lacunae from 13–30 to 16–00, respectively, the dial of the clock; in these lacunae, the “tentacles” are located at the pupil. In the zone from 15-00 to 16-30 there are no spots + blurry spots along the autonomous ring. AK burst at 15-30, light brown spot “plugging” gap, ЛР. A group of small lacunas of dark blue color at 15-00 to 16-00. The absence of stains, but the presence of a distinct large lacuna in the desired area suggests the success of the treatment. Non-palpable FCM does not give signs. The most significant case is presented in Fig. 1

The figure shows the iris of a patient with fibroadenoma. Clearly detected spots in the area – 15.00, one more clear, and there is a blurred area in the region of 15-16.30. There are spots all over the iris. The presence of obvious signs on the two irises and on one of them is the predominance of spots by area than other spots.
In patients with breast cancer BI, the following changes were found on the iris of the eye: angle (indentation) AK 15-20 and a dark large spot in the lacuna behind it. A group of small lacunae of dark blue color at 15-00 to 16-00, and from 14-00 to 15-00. Inset group of lacunae triangle from 15-00 to 15-30, the angle of the lacunae at 14-45, the lacuna is dark blue at the back. LR, two corners of the lacunas at 14-00 and 15-50, in one of them 2 lacunas of dark blue color. Lacuna at 15-00 to 15-30 with a small gap AK for 15-15 to 15-30, and the flow of lacunae from 14-00 to 14-30. Lacuna at 15-30 with dark spots in it with a gap AK, a triangle at 14-30.
In this group of patients, the most pronounced changes in the iris characteristic for breast cancer are shown in Fig.2. The angle (indentation) of the AK by 15–20 and a dark large spot in the lacuna behind it are revealed.
Fig.2. Patient No. 4 is the most significant case of breast cancer.

For patients from the breast cancer group B12, characteristic changes in the iris were: a spot in the zone – 15.00, a blurred zone in the region of 15-16.30 in area, exceeding the other spots of the iris. The presence of obvious signs on the two irises and on one of them is the predominance of spots by area than other spots. Bright spot + less obvious in the area of 15.0016.30. The accumulation of large lacunae from 13-30 to 16-00 with “tentacles” at the pupil in a brown background. Burst AK at 15-00 with a small lacuna inside. A small spot in one of the iris in the desired area of presence suggests the presence of the disease, but it does not exceed other spots on the same iris and in terms of color and area saturation. Dark blue background at 14-30 – a sign of a chronic disease.
The most striking example of this group of patients is presented in Fig.3. The figure clearly shows the AK gap at 1515 with the presence of a brown spot at 15-30, followed by fibrillation.
Fig.3. Patient No. 16 is an indicative case in group E12.

The BC13 B13 group is represented by one patient (Fig. 4). She has a pyramidal lacuna on the iris from 2000 to 20-45 with an AK gap, with a light portion in the AK, with a spot inside, a clear lacuna at 15-30, there are no more such lacunae.
Fig.4. Patient number 34 – signs of breast cancer B13

In the last studied group, the desired changes in the iris were detected only in one patient (Fig.5). This patient has several spots in 15-16.30 + spots in a circle from 15-21. The presence of bright saturation spots on the left iris and the presence of spots on both irises in the desired areas indicates the presence of obvious signs of the presence of the disease, the angle of the gaps at 14-45. The iris is deployed due to the inclination of the head, the angle of the lacunas. Gap AK at 15-00 to 16-00, a group of lacunas at 14-00 rushing to the pupil.
Results and their discussion: With FCM and breast fibroadenoma, this diagnostic method is specific in 80%. In 34 out of 34 women, iridodiagnostic signs were detected in 29, which is 85%. Thus, the method of iridology allows to identify the pathology of the breast. In the group of patients with St1 breast cancer out of 12 people, changes were found in 10, which is 83%; with breast cancer St2 of 17 patients – in 15 (88.2%); in the group with breast cancer St3, there is only one patient, therefore the detection of pathology was 100%; in the breast cancer group, St4 out of 4 patients revealed pathology in one woman (25%). This method in non-malignant tumors of the breast is defined as changes in the iris common with changes in breast cancer, and in breast cancer there are specific changes, namely, the angles from the lacunae, the insertion of the lacunae group of triangles, the indentation of AK.
Conclusions: 1. The use of iridology in the outpatient setting for screening patients with breast cancer in the early stages can be a valuable rapid diagnostic method. According to our data, the method is specific in the diagnosis of breast cancer in 85% of cases, and when FCM is detected, in 80% of cases. In the early stages of diagnosis, pathology without treatment is better detected than after treatment. Pathology detection after treatment was only 25%.
2. Differential diagnosis using iridology between malignant and benign tumors is possible, but only in the presence of clear signs of malignancy. In other cases, differentiating tumors without additional methods of examining patients is difficult.
3. To improve the accuracy of the research method, photographic equipment of a higher technological level is necessary, which, due to its high cost, prevents the introduction into wide practice as a method for diagnosing the pathology of the mammary glands.
Literature.
1. Avdeeva O. S., Ivleva N. N., Ivakhina S. A. Changes in the human iris in connection with pathological changes in organs and tissues. // Medical web conferencing newsletter. – 2016. – Т.6, №5. – P.709.
2. Axel E.M. Malignant tumors of the breast. The state of cancer care, morbidity and mortality // Mammology. – 2006. – №1. – P.9-15.
3. Aleksandrova L.M .; Sotnikova E.N .; Vilkov-Belenko E.S .; Leonov N.V .; Veize D.L. Method for rapid diagnosis of thyroid adenoma // Patent of the Russian Federation. – 1997.
4. Borsukov A.V., Soloviev V.I. // Malignant tumors – 2013. – №2. – pp. 1667-168.
5. Daljanov BM, Iskandarova MA, Rasulova KA, Iskandarov AI Iridodiagnostics in the service of forensic medicine // Europaische fachhochschule. – 2014. – N5. – P.29-31.
6. Volovar OS, Malanchuk VO, Tsilenko OL, Kryzhanivska OO Iridodiagnostics in maxillofacial surgery // Novini dentists. – 2010. – N4. – P.25-30.
UDC: 616-008
Full Russian Abstract: Download